Heart failure develops when the heart, via an abnormality of cardiac function (detectable or not), fails to pump blood at a rate commensurate with the requirements of the metabolizing tissues or is able to do so only with an elevated diastolic filling pressure, associated with pulmonary wedge congestion and elevated PCWP.

Signs and symptoms
Signs and symptoms of heart failure:
The New York Heart Association (NYHA) classification system categorizes heart failure on a scale of I to IV, as follows:
- Class I: No limitation of physical activity
- Class II: Slight limitation of physical activity
- Class III: Marked limitation of physical activity
- Class IV: Symptoms occur even at rest; discomfort with any physical activity
The American College of Cardiology/American Heart Association (ACC/AHA) staging system is defined by the following four stages :
- Stage A: High risk of heart failure but no structural heart disease or symptoms of heart failure
- Stage B: Structural heart disease but no symptoms of heart failure
- Stage C: Structural heart disease and symptoms of heart failure
- Stage D: Refractory heart failure requiring specialized interventions
The following tests may be useful in the initial evaluation for suspected heart failure :
Complete blood count (CBC), Iron studies, Urinalysis, Electrolyte levels, Renal and liver function studies, Fasting blood glucose levels, Lipid profile, Thyroid stimulating hormone (TSH) levels, B-type natriuretic peptide levels, N-terminal pro-B-type natriuretic peptide levels, Electrocardiography, Chest radiography, Two-dimensional (2-D) echocardiography, Nuclear imaging , Maximal exercise testing, Pulse oximetry or arterial blood gas.
Background
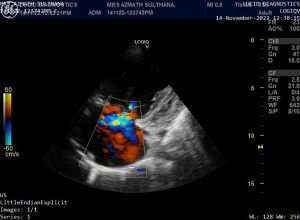
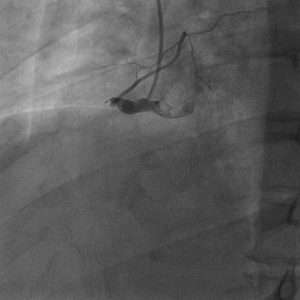
Heart failure (see the images below) may be caused by myocardial failure but may also occur in the presence of near-normal cardiac function under conditions of high demand. Heart failure always causes circulatory failure, but the converse is not necessarily the case, because various noncardiac conditions (eg, hypovolemic shock, septic shock) can produce circulatory failure in the presence of normal, modestly impaired, or even supra normal cardiac function. To maintain the pumping function of the heart, compensatory mechanisms increase blood volume, cardiac filling pressure, heart rate, and cardiac muscle mass. However, despite these mechanisms, there is a progressive decline in the ability of the heart to contract and relax, resulting in worsening heart failure.
Etiology
Most patients who present with significant heart failure do so because of an inability to provide adequate cardiac output in that scenario. This is often a combination of the causes listed below in the setting of an abnormal myocardium. The list of causes responsible for presentation of a patient with heart failure exacerbation is very long, and searching for the proximate cause to optimize therapeutic interventions is important.
From a clinical standpoint, classifying the causes of heart failure into the following four broad categories is useful:
- Underlying causes: Underlying causes of heart failure include structural abnormalities (congenital or acquired) that affect the peripheral and coronary arterial circulation, pericardium, myocardium, or cardiac valves, thus leading to increased hemodynamic burden or myocardial or coronary insufficiency
- Fundamental causes: Fundamental causes include biochemical and physiologic mechanisms, through which either an increased hemodynamic burden or a reduction in oxygen delivery to the myocardium results in impairment of myocardial contraction
- Precipitating causes: Overt heart failure may be precipitated by progression of the underlying heart disease (eg, further narrowing of a stenotic aortic valve or mitral valve) or various conditions (fever, anemia, infection) or medications (chemotherapy, nonsteroidal anti-inflammatory drugs [NSAIDs]) that alter the homeostasis of heart failure patients
- Genetics of cardiomyopathy: Dilated, arrhythmic right ventricular and restrictive cardiomyopathies are known genetic causes of heart failure
Myocytes and myocardial remodeling
In the failing heart, increased myocardial volume is characterized by larger myocytes approaching the end of their life cycle. As more myocytes drop out, an increased load is placed on the remaining myocardium, and this unfavorable environment is transmitted to the progenitor cells responsible for replacing lost myocytes.
Progenitor cells become progressively less effective as the underlying pathologic process worsens and myocardial failure accelerates. These features—namely, the increased myocardial volume and mass, along with a net loss of myocytes—are the hallmark of myocardial remodeling. This remodeling process leads to early adaptive mechanisms, such as augmentation of stroke volume (Frank-Starling mechanism) and decreased wall stress (Laplace law) and, later, to maladaptive mechanisms such as increased myocardial oxygen demand, myocardial ischemia, impaired contractility, and arrhythmogenesis.
As heart failure advances, there is a relative decline in the counterregulatory effects of endogenous vasodilators, including nitric oxide (NO), prostaglandins (PGs), bradykinin (BK), atrial natriuretic peptide (ANP), and B-type natriuretic peptide (BNP). This decline occurs simultaneously with the increase in vasoconstrictor substances from the RAAS and the adrenergic system, which fosters further increases in vasoconstriction and thus preload and afterload. This results in cellular proliferation, adverse myocardial remodeling, and anti natriuresis, with total body fluid excess and worsening of heart failure symptoms.
Systolic and diastolic failure
Systolic and diastolic heart failure each result in a decrease in stroke volume. This leads to activation of peripheral and central baroreflexes and chemoreflexes that are capable of eliciting marked increases in sympathetic nerve traffic.
Although there are commonalities in the neurohormonal responses to decreased stroke volume, the neurohormone-mediated events that follow have been most clearly elucidated for individuals with systolic heart failure. The ensuing elevation in plasma norepinephrine directly correlates with the degree of cardiac dysfunction and has significant prognostic implications. Norepinephrine, while directly toxic to cardiac myocytes, is also responsible for a variety of signal-transduction abnormalities, such as downregulation of beta1-adrenergic receptors, uncoupling of beta2-adrenergic receptors, and increased activity of inhibitory G-protein. Changes in beta1-adrenergic receptors result in overexpression and promote myocardial hypertrophy.

Underlying causes of systolic heart failure include the following: Coronary artery disease, Diabetes mellitus, Hypertension, Valvular heart disease (stenosis or regurgitant lesions), Arrhythmia (supraventricular or ventricular), Infections and inflammation (myocarditis), Peripartum cardiomyopathy, Congenital heart disease, Drugs (either recreational, such as alcohol and cocaine, or therapeutic drugs with cardiac side effects, such as doxorubicin), Idiopathic cardiomyopathy, Rare conditions (endocrine abnormalities, rheumatologic disease, neuromuscular conditions).
Underlying causes of diastolic heart failure include the following: Coronary artery disease, Diabetes mellitus, Hypertension, Valvular heart disease (aortic stenosis), Hypertrophic cardiomyopathy, Restrictive cardiomyopathy (amyloidosis, sarcoidosis), and Constrictive pericarditis.
Underlying causes of acute heart failure include the following: Acute valvular (mitral or aortic) regurgitation, Myocardial infarction (MI), Myocarditis, Arrhythmia, Drugs (eg, cocaine, calcium channel blockers, or beta-blocker overdose), and Sepsis.
Underlying causes of high-output heart failure include the following: Anemia, Systemic arteriovenous fistulas, Hyperthyroidism, Beriberi heart disease, Paget disease of bone, Albright syndrome (fibrous dysplasia), Multiple myeloma, Pregnancy, Glomerulonephritis, Polycythemia vera, and Carcinoid syndrome
Underlying causes of right heart failure include the following: LV failure, Coronary artery disease (ischemia), Pulmonary hypertension, Pulmonary valve stenosis, Pulmonary embolism, Chronic pulmonary disease, and Neuromuscular diseases.
Genetics of cardiomyopathy
Autosomal dominant inheritance has been demonstrated in dilated cardiomyopathy and in arrhythmic right ventricular cardiomyopathy. Restrictive cardiomyopathies are usually sporadic and associated with the gene for cardiac troponin I. Genetic tests are available at major genetic centers for cardiomyopathies.
In families with a first-degree relative who has been diagnosed with a cardiomyopathy leading to heart failure, the at-risk patient should be screened and followed. The recommended screening consists of an electrocardiogram and an echocardiogram. If the patient has an asymptomatic LV dysfunction, it should be documented and treated.
Men and women have a similar incidence and prevalence of heart failure. However, many differences remain between men and women with heart failure, such as the following:
- Whereas the incidence of heart failure in men approximately doubles with each 10-year age increase between 65 and 85 years, it triples for women between ages 65 to 74 years and 75 to 85 years
- Women tend to develop heart failure later in life than men do
- Women are more likely than men to have preserved systolic function
- Women develop depression more commonly than men do
- Women have signs and symptoms of heart failure similar to those of men, but they are more pronounced in women
- Women survive longer with heart failure than men do
The prevalence of heart failure increases with age. The prevalence is 1-2% of the population younger than 55 years and increases to a rate of 10% for persons older than 75 years. Nonetheless, heart failure can occur at any age, depending on the cause.
Management
Treatment includes the following:
- Nonpharmacologic therapy: Oxygen and noninvasive positive pressure ventilation, dietary sodium and fluid restriction, physical activity as appropriate, and attention to weight gain
- Pharmacotherapy: Diuretics, vasodilators, inotropic agents, anticoagulants, beta blockers, ACE inhibitors, ARBs, CCBs, digoxin, nitrates, B-type natriuretic peptids, I(f) inhibitors, ARNIs, and soluble guanylate cyclase stimulators
Surgical options
Surgical treatment options include the following:
- Electrophysiologic intervention
- Revascularization procedures
- Valve replacement/repair
- Ventricular restoration
- Extracorporeal membrane oxygenation
- Ventricular assist devices
- Heart transplantation
- Total artificial heart
Prognosis
In general, the mortality following hospitalization for patients with heart failure is 10.4% at 30 days, 22% at 1 year, and 42.3% at 5 years, despite marked improvement in medical and device therapy.
Mortality is greater than 50% for patients with New York Heart Association (NYHA) class IV, American College of Cardiology/American Heart Association (ACC/AHA) stage D heart failure. Heart failure associated with acute myocardial infarction (MI) has an inpatient mortality of 20-40%; mortality approaches 80% in patients who are also hypotensive (eg, cardiogenic shock).
contact: dramthirugnanam@gmail.com







Best view i have ever seen !
Best View i have ever seen !
Hi there to every one, it’s actually a good for me to go to see
this web page, it consists of useful Information.
Best view i have ever seen !
Best view i have ever seen !
Hey! This is my first comment here so I just wanted to give a quick shout out and say I truly enjoy reading your articles. Can you recommend any other blogs/websites/forums that go over the same subjects? Thank you!
Best views i have ever seen !
Hi! I’ve been following your web site for a while now and finally got the courage to go ahead and give you a shout out from Austin Tx! Just wanted to mention keep up the good work!
Do you mind if I quote a few of your posts as long as I provide credit and sources back to your weblog? My blog site is in the very same area of interest as yours and my users would really benefit from a lot of the information you present here. Please let me know if this okay with you. Appreciate it!
You are my breathing in, I possess few web logs and rarely run out from brand :). “He who controls the past commands the future. He who commands the future conquers the past.” by George Orwell.
Some truly nice and useful info on this web site, as well I think the design has got wonderful features.
I conceive this site has got very fantastic composed content material content.
At this time it seems like WordPress is the top blogging platform available right now. (from what I’ve read) Is that what you’re using on your blog?
Thanks, I’ve just been looking for info about this topic for a long time and yours is the greatest I’ve discovered so far. However, what concerning the conclusion? Are you positive concerning the supply?
My spouse and i felt absolutely satisfied when Emmanuel managed to carry out his web research because of the precious recommendations he made while using the site. It’s not at all simplistic to simply be offering techniques which often many people may have been making money from. And now we realize we have got the blog owner to appreciate for this. The most important explanations you’ve made, the straightforward website menu, the friendships you make it easier to promote – it’s got everything great, and it’s letting our son in addition to our family believe that the article is entertaining, and that is extremely vital. Many thanks for all the pieces!
I haven?¦t checked in here for a while because I thought it was getting boring, but the last few posts are good quality so I guess I?¦ll add you back to my daily bloglist. You deserve it my friend 🙂
Thank you for the sensible critique. Me and my neighbor were just preparing to do a little research on this. We got a grab a book from our area library but I think I learned more clear from this post. I’m very glad to see such wonderful info being shared freely out there.
Wonderful site you have here but I was wondering if you knew of any user discussion forums that cover the same topics discussed in this article? I’d really like to be a part of group where I can get feedback from other experienced individuals that share the same interest. If you have any suggestions, please let me know. Many thanks!
It¦s truly a nice and helpful piece of info. I am satisfied that you shared this helpful info with us. Please stay us up to date like this. Thanks for sharing.
You could certainly see your skills in the work you write. The arena hopes for even more passionate writers like you who aren’t afraid to mention how they believe. Always follow your heart.
This is the right blog for anyone who wants to find out about this topic. You realize so much its almost hard to argue with you (not that I actually would want…HaHa). You definitely put a new spin on a topic thats been written about for years. Great stuff, just great!
Do you mind if I quote a couple of your articles as long as I provide credit and sources back to your site? My blog site is in the exact same area of interest as yours and my visitors would really benefit from a lot of the information you provide here. Please let me know if this ok with you. Thanks a lot!
ofcourse sir
I have recently started a website, the information you offer on this web site has helped me greatly. Thanks for all of your time & work.
I do trust all the concepts you’ve introduced in your post.
They’re really convincing and can definitely work. Still, the posts are very brief for
newbies. May you please lengthen them a little from subsequent time?
Thank you for the post.
Reading your article has greatly helped me, and I agree with you. But I still have some questions. Can you help me? I will pay attention to your answer. thank you.
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me? https://www.binance.com/tr/register?ref=PORL8W0Z
Your article gave me a lot of inspiration, I hope you can explain your point of view in more detail, because I have some doubts, thank you.
Your article gave me a lot of inspiration, I hope you can explain your point of view in more detail, because I have some doubts, thank you.
Thank you very much for sharing, I learned a lot from your article. Very cool. Thanks. nimabi
Thank you very much for sharing, I learned a lot from your article. Very cool. Thanks. nimabi