Introduction
Primary Pulmonary Artery Hypertension or Idiopathic pulmonary arterial hypertension (IPAH) is a rare disease characterized by elevated pulmonary artery pressure with no apparent cause. PPHTN is also termed WHO Group I pulmonary hypertension (PH), precapillary pulmonary hypertension, and, previously, primary pulmonary hypertension. Untreated, IPAH leads to right-sided heart failure and left heart failure and eventually to death.
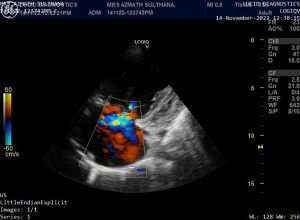
Echocardiogram Findings
The echocardiogram findings may or may not demonstrate the presence of a pericardial effusion. In approximately a third of patients with pulmonary arterial hypertension (PAH), Doppler echocardiography sometimes demonstrates right-to-left shunting across a patent foramen ovale, enlargement of right ventricle, right atrium, main pulmonary artery and inferior vena cava and inter ventricular septum deviation towards left ventricle.

Signs and Symptoms of PPHTN
Symptoms of PPHTN are nonspecific and commonly include the following:
- Dyspnea
- Fatigue
- Weakness
- Syncope or presyncope
- Occasional chest pain
Cardiovascular examination in patients with PAH often reveals the following findings:
- The pulmonic component of the second heart sound is usually increased, which may demonstrate fixed or paradoxical splitting in the presence of severe right ventricular dysfunction; occasionally, the second heart sound may be palpable
- A pulmonic regurgitation (Graham Steell murmur) may be apparent
- A murmur of tricuspid regurgitation can be present, and a right ventricular lift (heave) may be noted
- Jugular venous pulsations may be elevated in the presence of volume overload, right ventricular failure, or both; large V waves are often present because of the commonly present severe tricuspid regurgitation, and large a waves thought to be secondary to poor right ventricular compliance may also be present
- Right-sided S3 gallop
Other findings may include the following:
- Hepatomegaly with palpable pulsations of the liver
- Abnormal abdominal-jugular reflex
- Ascites – Not uncommon in untreated patients and in patients with worsening decompensated right heart failure
- Pitting edema – In the extremities
- Presacral edema – In patients who are bedridden
Diagnosis and Investigations
Cardiac catheterization
Cardiac catheterization is the criterion standard test to definitively confirm any form of PAH. It is essential in the workup of all patients suspected of IPAH. Excluding left-sided heart disease, including diastolic dysfunction, is especially important in these patients because of major treatment implications. Catheterization is also performed to determine pulmonary vasoreactivity, which can be prognostic and figures in the initiation and titration of high-dose calcium channel blocker (CCB) therapy.
Laboratory studies
Antinuclear antibody
D-Dimer
Uric acid
Thyroid function
B-type natriuretic peptide, or N-terminal B-type natriuretic peptide
Pulmonary function testing (PFT)
Imaging studies – Essential
Chest radiography: A chest radiograph may help identify secondary causes of, or contributors to, pulmonary hypertension.
Echocardiography: The echocardiogram can estimate right ventricular (RV) systolic pressure and, more importantly, the degree of right ventricular enlargement, as well as the presence of a pericardial effusion. Equally important, the echocardiogram helps to exclude secondary causes of, or contributors to, pulmonary hypertension, such as left-sided heart disease (eg, left ventricular dysfunction, valvular heart disease).
Nuclear lung ventilation/perfusion scanning: This is performed to exclude chronic thromboembolic pulmonary hypertension (Group IV PH).
Imaging studies – Conditional
Chest computed tomography (CT)
Magnetic resonance imaging (MRI)
Pulmonary angiography
Electrocardiography
Electrocardiographic results are often abnormal in patients with PAH, revealing right atrial enlargement, right axis deviation, right ventricular hypertrophy, and characteristic ST depression and T-wave inversions in the anterior leads. Sometimes, an incomplete RBBB may be seen (usually in patients with atrial septal defects). However, some patients with IPAH have few or no abnormal electrocardiographic findings.
Histology
Several histologic subtypes are associated with pulmonary arteriopathy in IPAH, including plexogenic arteriopathy, in situ thrombosis, and intimal and adventitial proliferation.
Exercise testing
In patients with IPAH, values for peak exercise oxygen consumption, oxygen pulse, and ventilator equivalents (ratio of expired volume to carbon dioxide output [ie, wasted ventilation fraction] at the anaerobic threshold) during exercise are abnormal to varying degrees.
Commonly, a 6-minute walk test is performed in the office as a crude measurement of exercise capacity.
Treatment and Management
Calcium channel blocker therapy
Only in a small subset of PPHTN patients, long-term treatment results in clinical improvement; this is in patients who are proven responders to calcium channel blockers (CCBs) and do not have contraindications to CCBs (depressed cardiac output and/or systemic hypotension). In general, CCBs are used at high doses in patients with PPHTN.
PAH-specific therapy
For patients with PPHTN in whom CCBs are contraindicated (most IPAH patients), or in whom CCBs are ineffective or poorly tolerated, guidelines from the joint European Respiratory Society (ERS)/European Society of Cardiology (ESC) recommend using the patient’s World Health Organization (WHO) functional class to guide the choice of PAH-specific therapy.
More comprehensive guidelines encompass several clinical parameters that are used to determine risk of adverse outcomes. These include functional class, exercise capacity, symptom progression rate, the presence or absence of heart failure on examination, certain biomarkers, and findings on echocardiography.
Parenteral Prostanoids
Class Summary
Parenteral Prostanoids are used for patients whose IPAH fails to respond to calcium channel blockers or who cannot tolerate these agents and who have New York Heart Association (NYHA) type III or IV right-sided heart failure.
Epoprostenol
An analogue of aerosolized prostacyclin (PGI2) that was approved by the FDA in 1995 for use in patients with IPAH, and later for use in APAH, epoprostenol has potent vasodilatory properties, an immediate onset of action, and a half-life of approximately 5 min. In addition to its vasodilator properties, this agent also contributes to inhibition of platelet aggregation and plays a role in inhibition of smooth muscle proliferation. The latter effect may have implications for beneficial remodeling of pulmonary vascular bed. Epoprostenol is FDA-approved for treatment of IPAH.
Treprostinil (Remodulin)
The prostanoid, treprostinil is used to treat PAH. It is structurally similar to epoprostenol but stable at room temperature and has a longer half-life; therefore, it can be given as an intravenous or subcutaneous continuous infusion via a smaller pump. This agent elicits direct vasodilation of pulmonary and systemic arterial vessels and inhibits platelet aggregation. Vasodilation reduces right and left ventricular afterload and increases cardiac output and stroke volume.
Treprostinil recently received FDA approval for IV use as a bioequivalent of subcutaneous treprostinil, using the same delivery pump used for epoprostenol. Dosing is similar to subcutaneous delivery.
Adenosine (Adenocard)
Adenosine is an antiarrhythmic agent that is used for the treatment of paroxysmal supraventricular tachycardia. It slows conduction time through the AV node, which can interrupt the re-entry pathways through the AV nodes, in turn restoring normal sinus rhythm.
Oral Phosphodiesterase (Type 5) Enzyme Inhibitors
Class Summary
Inhibition of the antiproliferative effects of the PDE-5 pathway, which regulates cyclic guanosine monophosphate hydrolysis, may be significant in the long-term treatment of pulmonary hypertension.
Despite concerns regarding ocular toxicity with chronic PDE-5 inhibition, no detrimental effects were observed during a pivotal phase III randomized clinical trial of sildenafil versus placebo for patients with pulmonary arterial hypertension.
A 52-week extension study demonstrated the long-term safety and efficacy of tadalafil in patients with pulmonary arterial hypertension.
Sildenafil (Revatio)
Sildenafil promotes selective smooth muscle relaxation in lung vasculature, possibly by inhibiting PDE-5. This results in subsequent reduction of blood pressure in pulmonary arteries and an increase in cardiac output.
Tadalafil (Adcirca)
Tadalafil is a PDE-5 inhibitor indicated for improving and increasing exercise capacity in patients with World Health Organization (WHO) class I PAH. This agent increases cyclic guanosine monophosphate (cGMP), which is the final mediator in the nitric oxide pathway.
Inhaled Prostanoids
Class Summary
Inhaled prostacyclin (PGI2) synthetic analogues are an alternative to parenteral administration. They are used in an attempt to limit systemic adverse effects.
Iloprost (Ventavis)
A synthetic analogue of PGI2 that dilates systemic and pulmonary arterial vascular beds, iloprost is indicated for WHO class I PAH in patients with NYHA class III or IV symptoms to improve exercise tolerance and symptoms and to delay deterioration.
Treprostinil inhaled (Tyvaso, Tyvaso)
The prostanoid, treprostinil is indicated for PAH in patients with NYHA class III symptoms. It elicits direct vasodilation of pulmonary and systemic arterial vessels and inhibits platelet aggregation. Vasodilation reduces right and left ventricular afterload and increases cardiac output and stroke volume.
Endothelin Receptor Antagonists
Class Summary
Endothelin receptor antagonists (ERAs) are therapeutic alternatives to parenteral prostacyclin agents. Given orally, they competitively bind to endothelin 1 (ET-1) receptors endothelin-A and endothelin-B, causing a reduction in pulmonary artery pressure (PAP), pulmonary vascular resistance (PVR), and mean right atrial pressure (RAP). This agent is indicated for treatment of PAH in patients with WHO class III or IV symptoms to improve exercise ability and decrease the rate of clinical deterioration.
Bosentan (Tracleer)
The first oral IPAH therapy to be approved in United States, Bosentan is a mixed endothelin-A and endothelin-B receptor antagonist indicated for PAH, including IPAH. In clinical trials, Bosentan improved exercise capacity, decreased the rate of clinical deterioration, improved functional class, and improved hemodynamics.
Bosentan improves pulmonary arterial hemodynamics by competitively binding to ET-1 receptors endothelin-A and endothelin-B in pulmonary vascular endothelium and pulmonary vascular smooth muscle. This leads to a significant increase in the cardiac index associated with a significant reduction in PAP, PVR, and mean RAP. These changes result in an improvement in exercise capacity (as measured by the 6-min walk test) and improved PAH symptoms.
Because this drug has teratogenic potential and because of the need for careful scrutiny in choosing appropriate candidates for ERA therapy, bosentan can be prescribed only through the Tracleer Access Program. Call 1-866-228-3546.
Ambrisentan (Letairis)
Ambrisentan is an endothelin receptor antagonist indicated for WHO group 1 PAH to 1) improve exercise ability and delay clinical worsening; and 2) in combination with tadalafil to reduce the risks of disease progression and hospitalization for worsening PAH, and to improve exercise ability. It inhibits vessel constriction and elevation of blood pressure by competitively binding to endothelin-1 receptors ETA and ETB in endothelium and vascular smooth muscle.
Diuretics
Class Summary
Diuretics are used in pulmonary hypertension to manage peripheral edema. The use of loop diuretics (e.g.-furosemide, bumetanide) requires potassium supplementation and close monitoring of serum potassium.
Furosemide (Lasix)
Furosemide is a loop diuretic that increases excretion of water by interfering with chloride-binding cotransport system, which in turn inhibits sodium and chloride reabsorption in ascending loop of Henle and distal renal tubule. It increases renal blood flow without increasing the filtration rate. It increases potassium, sodium, calcium, and magnesium excretion.
Diuretics have major clinical uses in managing disorders involving abnormal fluid retention (edema) or in treating hypertension, in which their diuretic action causes decreased blood volume.
Bumetanide
Bumetanide increases excretion of water by interfering with chloride-binding cotransport system, which, in turn, inhibits sodium, potassium, and chloride reabsorption in ascending loop of Henle. These effects increase urinary excretion of sodium, chloride, and water, resulting in profound diuresis. Renal vasodilation occurs following administration, renal vascular resistance decreases, and renal blood flow is enhanced.
Spironolactone
Spironolactone is a potassium-sparing diuretic. Potassium-sparing diuretics may have a role in ameliorating the sometimes-intractable hypokalemia observed with daily diuretic use.
Anticoagulants
Several studies, using both univariate and multivariate analyses, have shown that survival in IPAH, regardless of histopathologic subtype, is increased when patients are treated with anticoagulant therapy. However, these studies were retrospectively performed. No randomized, controlled clinical trials of anticoagulation in IPAH exist; thus, the data are mostly consensus-driven rather than based on prospective evidence-based medicine.
Warfarin should be used, provided the patient has no contraindications to anticoagulation. Maintain an international normalized ratio (INR) of 1.5 to 2.
Warfarin (Coumadin, Jantoven)
Warfarin interferes with hepatic synthesis of vitamin K–dependent coagulation factors. It is used for prophylaxis and treatment of venous thrombosis, pulmonary embolism, and thromboembolic disorders.
The efficacy of novel oral anticoagulants (NOACs) has not been evaluated in PAH.
Cardiac Glycosides
Digoxin therapy can be used to improve right ventricular function in patients with right ventricular failure. However, no randomized controlled clinical study has been performed to validate this strategy for patients with IPAH or any other form of PAH.
Digoxin (Lanoxin)
Digoxin enhances myocardial contractility by inhibition of Na+/K+ ATPase, a cell membrane enzyme that extrudes Na+ and brings K+ into the myocyte. It has direct inotropic effects in addition to indirect effects on the cardiovascular system. It increases myocardial systolic contractions and exerts vagomimetic action on sinus and AV nodes (slowing heart rate and conduction). Also, it decreases the degree of activation of sympathetic nervous system and renin-angiotensin system, which is referred to as the deactivating effect.
Transplantation and septostomy is the Final Care for the PPHTN.
- Lung transplantation – A single- or double-lung transplant is indicated for patients who do not respond to medical therapy
- Septostomy – Atrial septostomy is a palliative procedure that may afford some benefit to patients whose condition is deteriorating






Thank you very much for sharing, I learned a lot from your article. Very cool. Thanks. nimabi
Thanks for sharing. I read many of your blog posts, cool, your blog is very good. https://www.binance.info/en/join?ref=W0BCQMF1