Acute coronary syndrome (ACS) is a clinical presentation ranging from those for ST-segment elevation myocardial infarction (STEMI) to presentations found in non–ST-segment elevation myocardial infarction (NSTEMI) or in unstable angina. It is almost always associated with rupture of an atherosclerotic plaque and partial or complete thrombosis of the infarct-related artery. It causes a lot of mechanical damage to the heart if not treated early in the stage.
Signs and symptoms
Atherosclerosis is the primary cause of ACS, with most cases occurring from the disruption of a previously nonsevere lesion. Complaints reported by patients with ACS include the following:
- Palpitations
- Pain, which is usually described as pressure, squeezing, or a burning sensation across the precordium and may radiate to the neck, shoulder, jaw, back, upper abdomen, or either arm
- Exertional dyspnea that resolves with pain or rest
- Diaphoresis from sympathetic discharge
- Nausea from vagal stimulation
- Decreased exercise tolerance
Physical Findings
- Hypotension: Indicates ventricular dysfunction due to myocardial ischemia, myocardial infarction (MI), or acute valvular dysfunction
- Hypertension: May precipitate angina or reflect elevated catecholamine levels due to anxiety or to exogenous sympathomimetic stimulation
- Diaphoresis
- Pulmonary edema and other signs of left heart failure
- Extracardiac vascular disease
- Jugular venous distention
- Cool, clammy skin and diaphoresis in patients with cardiogenic shock
- A third heart sound (S3) and, frequently, a fourth heart sound (S4)
- A systolic murmur related to dynamic obstruction of the left ventricular outflow tract
- Rales on pulmonary examination (suggestive of left ventricular dysfunction or mitral regurgitation)
Diagnosis
Updated guidelines for the management of non-ST-segment elevation ACS were released in 2020 by the European Society of Cardiology (ESC). The updates place increased reliance on high-sensitivity cardiac troponin testing (hs-cTn) for diagnosis. The guidelines include the use of the CRUSADE risk score (Can Rapid risk stratification of Unstable angina patients Suppress ADverse outcomes with Early implementation) of the ACC/AHA guidelines.
In the emergency setting, electrocardiography (ECG) is the most important diagnostic test for angina. ECG changes that may be seen during anginal episodes include the following:
- Transient ST-segment elevations
- Dynamic T-wave changes: Inversions, normalizations, or hyperacute changes
- ST depressions: These may be junctional, downsloping, or horizontal
Laboratory studies that may be helpful include the following:
- Creatine kinase isoenzyme MB (CK-MB) levels
- Cardiac troponin levels
- Myoglobin levels
- Complete blood count
- Basic metabolic panel
Diagnostic imaging modalities that may be useful include the following:
- Chest radiography
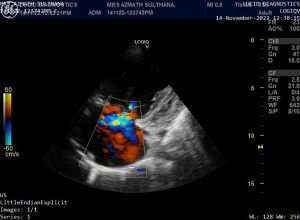
- Echocardiography
- Myocardial perfusion imaging
- Cardiac angiography
- Computed tomography, including CT coronary angiography and CT coronary artery calcium scoring
Treatment
Initial therapy must focus on the following:
- Stabilizing the patient’s condition
- Relieving ischemic pain
- Providing antithrombotic therapy
Pharmacologic anti-ischemic therapy includes the following:
- Nitrates (for symptomatic relief)
- Beta-blockers (eg, metoprolol): These are indicated in all patients unless contraindicated
- Flavinoids
Pharmacologic antithrombotic therapy includes the following:
- Aspirin
- Clopidogrel
- Prasugrel
- Ticagrelor
- Glycoprotein IIb/IIIa receptor antagonists (abciximab, eptifibatide, tirofiban)
Pharmacologic anticoagulant therapy includes the following:
- Unfractionated heparin (UFH)
- Low-molecular-weight heparin (LMWH; dalteparin, nadroparin, enoxaparin)
- Factor Xa inhibitors (rivaroxaban, fondaparinux)
Additional therapeutic measures that may be indicated include the following:
- Thrombolysis
- Percutaneous coronary intervention (preferred treatment for ST-elevation MI)
Current guidelines for patients with moderate- or high-risk ACS include the following:
- Early invasive approach
- Concomitant antithrombotic therapy, including aspirin and clopidogrel, as well as UFH or LMWH
Rehabilitation after Acute Coronary Syndrome
Patient education of risk factors is important, but more attention is needed regarding delays in door-to-balloon time, and one major barrier to improving this delay is patient education regarding his or her symptoms. Lack of recognition of symptoms may cause tremendous delays in seeking medical attention.
Educate patients about the dangers of cigarette smoking, a major risk factor for coronary artery disease (CAD). The risk of recurrent coronary events decreases by 50% 1 year after smoking cessation. Provide all patients who smoke with guidance, education, and support to avoid smoking. Smoking cessation classes should be offered to help patients avoid smoking after myocardial infarction. Bupropion increases the likelihood of successful smoking cessation.
Diet plays an important role in the development of CAD. Therefore, prior to hospital discharge, a patient who has had a myocardial infarction should be evaluated by a dietitian. Patients should be informed about the benefits of a low-cholesterol, low-salt diet. In addition, educate patients about AHA dietary guidelines regarding a low-fat, low-cholesterol diet.
A cardiac rehabilitation program after discharge may reinforce education and enhance compliance.
The following mnemonic may be useful in educating patients with CAD regarding treatments and lifestyle changes necessitated by their condition:
- A = Aspirin and antianginals
- B = Beta blockers and blood pressure (BP)
- C = Cholesterol and cigarettes
- D = Diet, and diabetes
- E = Exercise and education
For patients being discharged home, emphasize the following:
- Timely follow-up with a primary care provider
- Compliance with discharge medications, specifically aspirin and other medications used to control symptoms
- Need to return to the ED for any change in frequency or severity of symptoms







Very well written post. It will be useful to everyone who usess it, including yours truly :). Keep doing what you are doing – looking forward to more posts.
I’ve been exploring for a bit for any high quality articles or blog posts on this sort of area . Exploring in Yahoo I at last stumbled upon this website. Reading this information So i’m happy to convey that I have an incredibly good uncanny feeling I discovered just what I needed. I most certainly will make certain to don’t forget this website and give it a look regularly.
Good write-up, I’m normal visitor of one’s site, maintain up the nice operate, and It’s going to be a regular visitor for a long time.
This is a topic close to my heart cheers, where are your contact details though?
I may need your help. I tried many ways but couldn’t solve it, but after reading your article, I think you have a way to help me. I’m looking forward for your reply. Thanks.
I don’t think the title of your article matches the content lol. Just kidding, mainly because I had some doubts after reading the article. https://accounts.binance.com/bg/register-person?ref=RQUR4BEO
Your article gave me a lot of inspiration, I hope you can explain your point of view in more detail, because I have some doubts, thank you.
Your article gave me a lot of inspiration, I hope you can explain your point of view in more detail, because I have some doubts, thank you.
Your article gave me a lot of inspiration, I hope you can explain your point of view in more detail, because I have some doubts, thank you.